Anaphylaxis & Asthma
ANAPHYLAXIS
Anaphylaxis is a severe, potentially life-threatening allergic reaction. It can occur within seconds or minutes of exposure to something you're allergic to, such as peanuts or bee stings.
Anaphylaxis causes your immune system to release a flood of chemicals that can cause you to go into shock — your blood pressure drops suddenly and your airways narrow, blocking breathing. Signs and symptoms include a rapid, weak pulse; a skin rash; and nausea and vomiting. Common triggers include certain foods, some medications, insect venom and latex.
Anaphylaxis requires an injection of epinephrine and a follow-up trip to an emergency room. If you don't have epinephrine, you need to go to an emergency room immediately. If anaphylaxis isn't treated right away, it can be fatal.
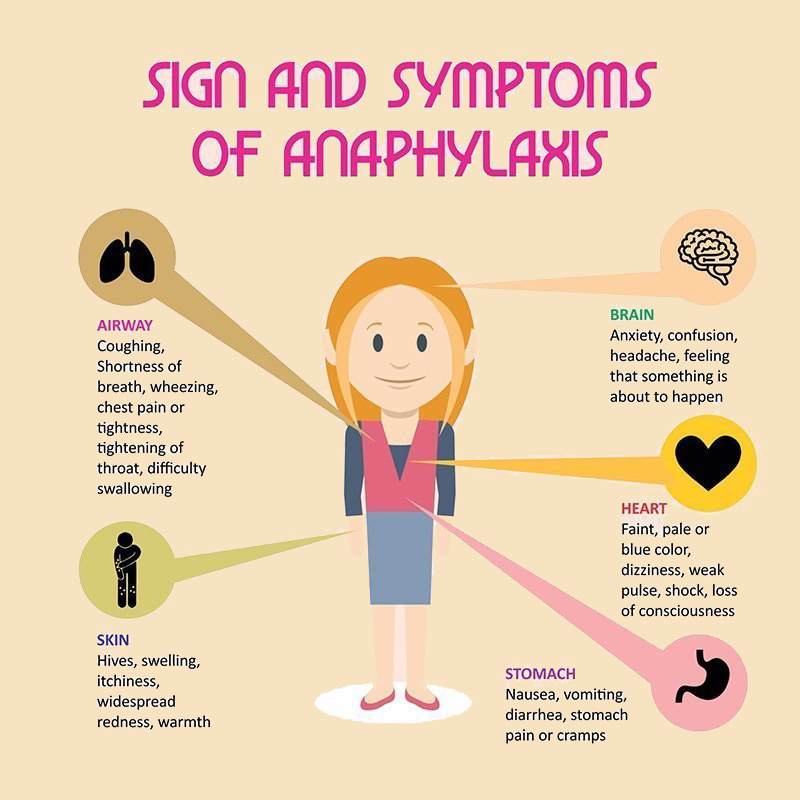
Symptoms
Anaphylaxis symptoms usually occur within minutes of exposure to an allergen. Sometimes, however, it can occur a half-hour or longer after exposure. Signs and symptoms include:
- Skin reactions, including hives and itching and flushed or pale skin
- Low blood pressure (hypotension)
- Constriction of your airways and a swollen tongue or throat, which can cause wheezing and trouble breathing
- A weak and rapid pulse
- Nausea, vomiting or diarrhea
- Dizziness or fainting
When to see a doctor
Seek emergency medical help if you, your child or someone else you're with has a severe allergic reaction. Don't wait to see if the symptoms go away.
If the person having the attack carries an epinephrine autoinjector, administer it right away. Even if symptoms improve after the injection, you still need to go to an emergency room to make sure symptoms don't recur, even without more exposure to your allergen. This second reaction is called biphasic anaphylaxis.
Make an appointment to see your doctor if you or your child has had a severe allergy attack or signs and symptoms of anaphylaxis in the past.
The diagnosis and long-term management of anaphylaxis are complicated, so you'll probably need to see a doctor who specializes in allergies and immunology.
Causes
Your immune system produces antibodies that defend against foreign substances. This is good when a foreign substance is harmful, such as certain bacteria or viruses. But some people's immune systems overreact to substances that don't normally cause an allergic reaction.
Allergy symptoms aren't usually life-threatening, but a severe allergic reaction can lead to anaphylaxis. Even if you or your child has had only a mild anaphylactic reaction in the past, there's a risk of more severe anaphylaxis after another exposure to the allergy-causing substance.
The most common anaphylaxis triggers in children are food allergies, such as to peanuts, and tree nuts, fish, shellfish and milk. Besides allergy to peanuts, nuts, fish and shellfish, anaphylaxis triggers in adults include:
- Certain medications, including antibiotics, aspirin and other over-the-counter pain relievers, and the intravenous (IV) contrast used in some imaging tests
- Stings from bees, yellow jackets, wasps, hornets and fire ants (more about Insect Sting Allergy HERE)
- Latex (more about Latex Allergy HERE)
Although not common, some people develop anaphylaxis from aerobic exercise, such as jogging, or even less intense physical activity, such as walking. Eating certain foods before exercise or exercising when the weather is hot, cold or humid also has been linked to anaphylaxis in some people. Talk with your doctor about precautions to take when exercising.
If you don't know what triggers your allergy attack, certain tests can help identify the allergen. In some cases, the cause of anaphylaxis is never identified (idiopathic anaphylaxis).
Risk factors
There aren't many known risk factors for anaphylaxis, but some things that might increase your risk include:
- Previous anaphylaxis. If you've had anaphylaxis once, your risk of having this serious reaction increases. Future reactions might be more severe than the first reaction.
- Allergies or asthma. People who have either condition are at increased risk of having anaphylaxis.
- Certain other conditions. These include heart disease and an abnormal accumulation of a certain type of white blood cell (mastocytosis).
Complications
An anaphylactic reaction can be life-threatening — it can stop your breathing or your heartbeat.
Prevention
The best way to prevent anaphylaxis is to avoid substances that cause this severe reaction. Also:
- Wear a medical alert necklace or bracelet to indicate you have an allergy to specific drugs or other substances.
- Keep an emergency kit with prescribed medications available at all times. Your doctor can advise you on the contents. If you have an epinephrine autoinjector, check the expiration date and be sure to refill your prescription before it expires.
- Be sure to alert all your doctors to medication reactions you've had.
- If you're allergic to stinging insects, use caution around them. Wear long-sleeved shirts and pants; don't walk barefoot on grass; avoid bright colors; don't wear perfumes, colognes or scented lotions; and don't drink from open soda cans outdoors. Stay calm when near a stinging insect. Move away slowly and avoid slapping at the insect.
- If you have food allergies, carefully read the labels of all the foods you buy and eat. Manufacturing processes can change, so it's important to periodically recheck the labels of foods you commonly eat.
When eating out, ask how each dish is prepared, and find out what ingredients it contains. Even small amounts of food you're allergic to can cause a serious reaction.
Be prepared
Even if you're careful, at some point you'll likely be exposed to what you're allergic to. Fortunately, you can respond quickly and effectively to an allergy emergency by knowing the signs and symptoms of an anaphylactic reaction and having a plan to quickly treat those symptoms.
ASTHMA
Asthma is a condition that causes breathing problems. Kids may cough, wheeze, or be short of breath. This happens because airways in the lungs get swollen, smaller, and filled with mucus.
Asthma is common in kids and teens, and tends to run in families. It can be mild or so severe that it gets in the way of daily activities.
With medicine and the right care plan, asthma symptoms can be managed so that kids and teens can do just about anything they want to do.
WHAT CAUSES ASTHMA?
No one knows exactly why some people develop asthma. Experts think it might be a combination of environmental factors and genes.
People with asthma may have a parent or other close relative with asthma. Those who are overweight may be more likely to have it.
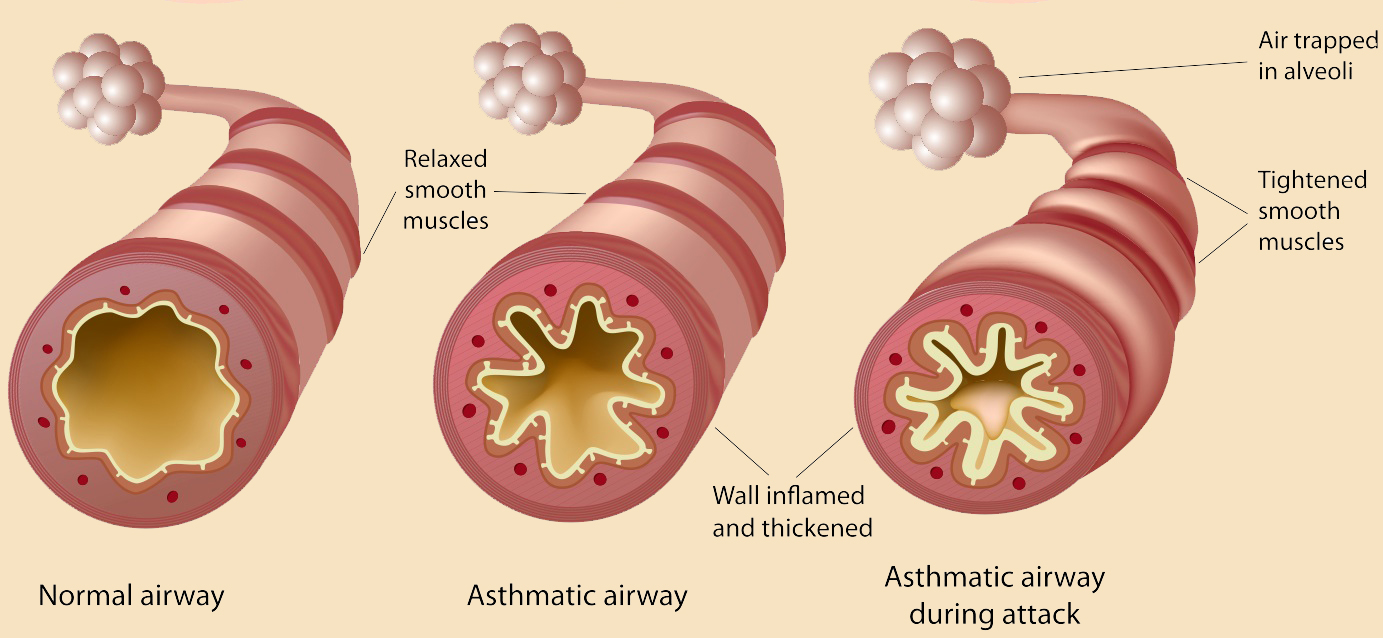
In asthma, air doesn't move through the lungs the way it should.
Normally, when someone breathes in, air goes in through the nose or mouth, down the windpipe (trachea), and into the airways (bronchioles) of the lungs. When people breathe out, air exits the body in the opposite direction.
With asthma, air has a harder time passing through. Airways swell and fill with mucus. The muscles around the airways tighten, making airways narrower. Things that can irritate the airways are called "triggers." Common triggers include cigarette smoke, allergies, and exercise.
Triggers can lead to asthma flare-ups or "attacks."
WHAT ARE THE SIGNS AND SYMPTOMS OF ASTHMA?
Flare ups are when asthma symptoms get worse. They happen when airways get more irritated and inflamed (swollen) than usual.
During a flare-up, kids might have:
- trouble breathing
- a tight chest
- a whistling sound while breathing (wheezing)
- a cough
- a fast heartbeat
Some flare-ups are serious, but others are mild. Flare-ups can happen suddenly or build up over time, especially if kids don't take their asthma medicines as directed.
Things that bring on a flare-up are called triggers. Triggers vary from person to person, but common ones include:
- allergies to things like pollen, mold, and pet dander
- irritants and pollutants in the air
- respiratory infections, like colds or flu
- weather conditions
- exercise (some kids only have asthma symptoms during or after exercise)
- gastroesophageal reflux
An important part of managing asthma is avoiding triggers. Your child's doctor will work with you to create a care plan that helps prevent flare-ups as much as possible.
HOW IS ASTHMA DIAGNOSED?
To diagnose asthma, doctors will ask questions about a child's health, problems with breathing, and family medical history. They'll also ask about any allergies, illnesses, and exposure to things that may make breathing worse.
Kids will have a physical exam and may have a lung function test. This usually involves testing breathing with a spirometer, a machine that analyzes airflow through the airways.
HOW IS ASTHMA TREATED?
There's no cure for asthma, but it can be managed to prevent flare-ups. Asthma treatment involves two important things: avoiding triggers and taking medicine.
Avoiding Triggers
There are many ways to avoid triggers. After your child's triggers are identified, the doctor will work with you to come up with a plan to avoid them.
For example, if pet dander or mold in your home trigger your child's asthma symptoms, you can make your home asthma-safe by changing the linens often, vacuuming regularly, and keeping the family pet out of your child's bedroom. If outdoor allergies (like pollen) are a problem, your child should avoid the outdoors on days when pollen counts are high.
If exercise is a trigger, the doctor may prescribe a medicine for your child to take before physical activity to prevent airways from tightening up. Doctors help people with exercise-induced asthma manage physical activity, not avoid it. Exercise can help people stay healthier overall (in fact, many pro athletes have asthma!).
Getting a yearly flu shot is also important, as illnesses like the flu can trigger asthma flare-ups.
Asthma Medicines
Most asthma medicines are breathed directly into the lungs (inhaled), but some are pills or liquids. There are two types of asthma medicines:
Quick-relief medicines act fast to open up tight airways. They can be used as needed during a flare-up. Quick-relief medicines act fast, but their effect doesn't last long. These kinds of medicines are also called "fast-acting" or "rescue" medicines.
Long-term control medicines manage asthma by preventing symptoms from happening. They reduce inflammation in the airways, which is the cause of the swelling and mucus. (Quick-relief medicines only treat the symptoms caused by the inflammation.) Long-term control medicines — also called "controller" or "maintenance" medicines — must be taken every day, even when kids feel well.
Some kids with asthma only need quick-relief medicine; others need both kinds of medicine to keep their asthma in check.
WHAT ELSE SHOULD I KNOW?
Asthma care can seem overwhelming, especially at first. But many tools are available to help you care for your child.
An asthma action plan is a care plan that you'll develop with the doctor. The plan gives detailed instructions on how to manage asthma, including:
- what medicines your child needs and when
- what your child's triggers are and how to avoid them
- how to manage a flare-up
- when to get emergency medical care
Following the plan can help your child do normal everyday activities without having asthma symptoms.
Keeping an asthma diary is another way to help manage asthma. Tracking your child's symptoms and medicines will help you know when your child is more likely to have a flare-up.
A peak-flow meter can help too. This handheld tool measures breathing ability. When peak flow readings drop, it's a sign of narrowing airways.
By using these tools, giving medicines as prescribed, and avoiding triggers, you'll help keep your child healthy and breathing well.
