Hand Eczema
Introduction
Hand eczema is one of the most common types of eczema (also referred to as ‘dermatitis’). It mainly affects the palms but can also affect other parts of the hand. The main symptoms are dry, itchy and red skin affecting the whole hand, including the fingers. Other symptoms may include cracking, soreness and bleeding. In some cases, blisters may develop. The skin is generally dry, scaly and thickened, and the fingers can become quite swollen when the eczema is flaring. If the eczema is severe over a long time, the hands can become very painful, making it difficult to carry out day-to-day tasks such as doing up buttons, holding a pen or using a computer.
The skin forms part of the immune system and helps to protect against infection. It not only provides a physical barrier, but the layers of skin contain specialised cells that destroy invading foreign proteins (antigens) such as bacteria and viruses. In people with eczema, the immune system overreacts in the skin, making it red and itchy.
Why does eczema appear on the hands?
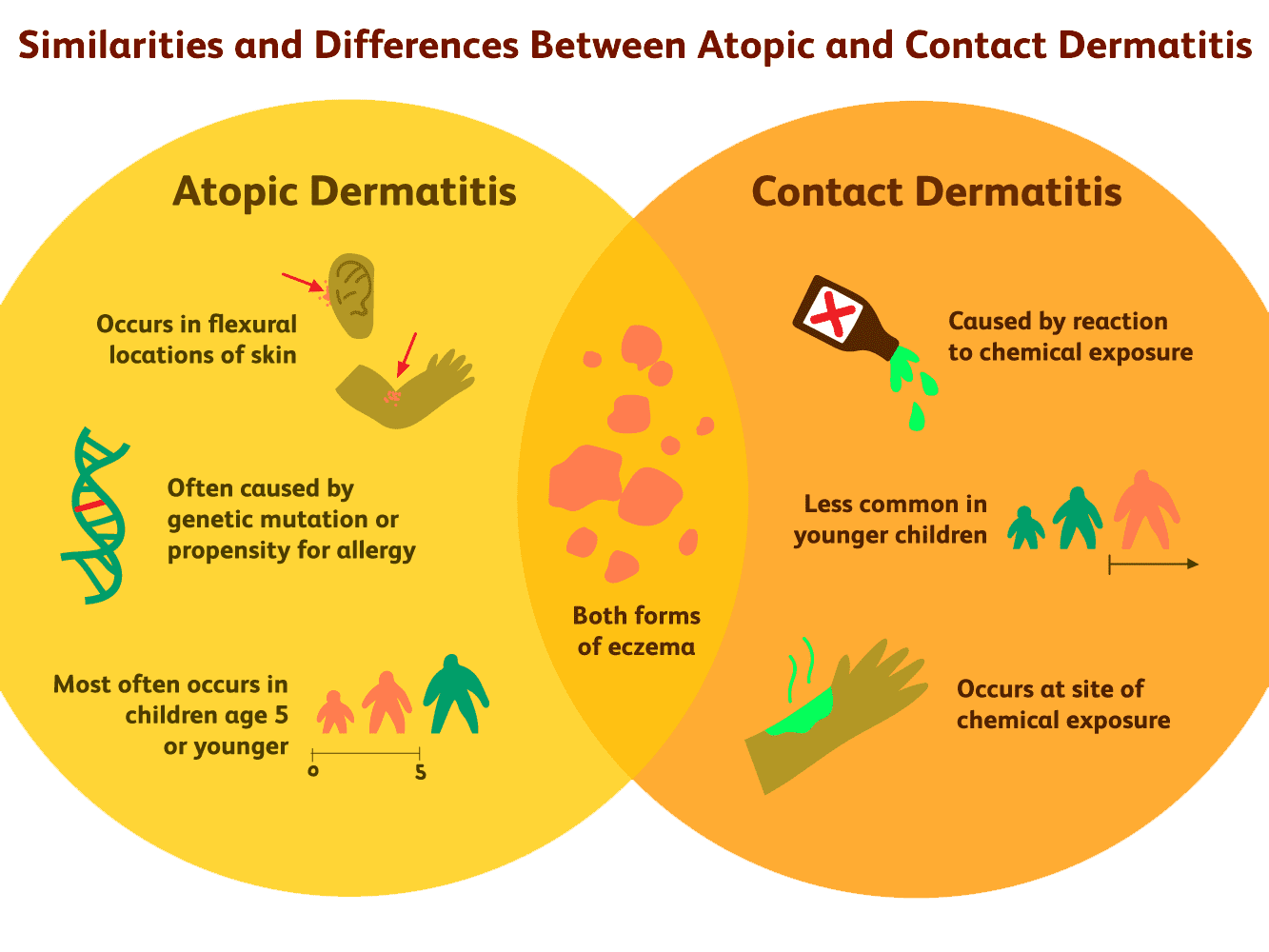
There can be a variety of reasons why eczema appears on the hands. For example, the hands can be affected by irritant or allergic contact dermatitis or both at the same time.
Coming into contact with irritants such as dust, detergents, cleaning agents, airborne sprays or even just frequent hand-washing can cause irritant hand eczema (irritant contact dermatitis of the hands). The skin on the palms of the hands is much thicker than elsewhere on the body (apart from the soles of the feet) and is normally able to withstand a great deal of wear and tear. But in people who regularly immerse their hands in detergents or solvents, the protective barrier of the skin breaks down, and eczema may develop. People who have this form of hand eczema often have a history of eczema in childhood.
Allergic hand eczema (allergic contact dermatitis of the hands) arises as a result of an allergic reaction to a particular substance in the environment. It is possible to be allergic to a number of different substances, but common causes of contact sensitivity include nickel, fragrances, preservative chemicals, rubber and various plants, amongst other things. Once a person’s immune system has identified a substance as ‘harmful’, they will react to the substance every time their skin is exposed to it, and this reaction becomes more severe on every exposure to the allergen.
When an allergic reaction of this kind is suspected, your GP should refer you to a dermatologist, who will normally perform patch tests to try to identify the allergic cause.
Pompholyx eczema (also known as dyshidrotic eczema/dermatitis) is another type of eczema that affects the hands (and feet). Usually pompholyx eczema involves the development of intensely itchy, watery blisters, mostly affecting the sides of the fingers, the palms of the hands and soles of the feet. Some people have pompholyx eczema on their hands and/or feet with other types of eczema elsewhere on the body. This condition can occur at any age but is most common before the age of 40 years.
The onset can be very sudden and the cause is unknown, although it is thought that factors such as stress, sensitivity to metal compounds (such as nickel, cobalt or chromate), heat and sweating can aggravate this condition. The skin is initially very itchy, and if you scratch, the blisters burst causing soreness and weeping. The skin will then dry out and often peel. Pompholyx can occur as an isolated event or may come and go in cycles.
How is hand eczema treated?
It is important to avoid any relevant irritants or allergens, and apply emollients and topical steroids as necessary.
Emollients
Emollients are medical moisturisers (creams, gels and ointments) that are available over-the-counter in pharmacies and on prescription. They should be used frequently throughout the day – even when the eczema is not active/flaring – to keep the skin moist and prevent it from drying out. Ointments are effective for very dry skin, but you might find them too greasy to use during the day. If so, use an ointment at night – under a pair of cotton gloves – and apply a cream frequently throughout the day. A leave-on emollient or an emollient soap substitute should be used for washing, since soap de-greases the skin and can also act as an irritant. It is a good idea to carry around a small pot of emollient to use for handwashing during the day, so you can avoid detergent hand washes.
Topical steroids
Topical steroids treat active eczema by reducing inflammation; this will reduce red, sore and cracked skin. Hands usually require stronger steroids (the skin of the palms is thick), so potent topical steroids are usually prescribed (moderately potent for children). They should be used for a short treatment burst, generally 2 weeks. If the skin is infected, you may be prescribed an antimicrobial treatment in the form of a cream or even a tablet.
Gloves
Wearing gloves may help to protect your hands from irritants and allergens, although you will still need to establish a good skincare routine using a soap substitute and an emollient cream or ointment. Ensure that the gloves give complete protection and that the insides remain dry. For general purposes and household tasks, rubber or PVC gloves with a cotton liner, or PVC gloves worn over cotton gloves, should suffice. Even when the eczema has cleared, the hands can remain very sensitive, so the use of cotton gloves within rubber gloves can be helpful when performing wet tasks.
Some jobs may recommend the use of barrier creams to protect employees’ hands. We would advise that people with hand eczema always use protective gloves (which should be provided by their workplace) and never barrier creams. Discuss any concerns with your Occupational Health department, who will provide the correct gloves for hand protection in the workplace.

What are the treatments for severe hand eczema?
If your hand eczema is severe, discuss the possibility of a dermatology referral with your GP. The referral may be for diagnosing contact allergy (patch testing) or for treatment, which may include a short course of oral steroids or immunosuppressants (e.g. azathioprine, ciclosporin, or methotrexate). Alternatively, dermatology departments may recommend alitretinoin (Toctino) or phototherapy, as described below.
Alitretinoin (Toctino)
Toctino is an oral treatment licensed for use in adults with severe chronic hand eczema that has not responded to treatment with potent topical steroids. Toctino is not known to be helpful for treating eczema on any other part of the body.
The active ingredient in Toctino is alitretinoin, a type of chemical that is naturally found in the body, and is known as a retinoid (as it is related to vitamin A). Toctino comes as a capsule in two strengths – 10 mg or 30 mg – and is taken once a day with a meal. Your doctor will decide which strength you need. Toctino has been shown to be effective in patients with severe hand eczema. It works by reducing the inflammation associated with eczema as well as damping down the response of the immune system. The treatment period is usually 12-24 weeks, depending on how your condition responds to this treatment.
SIDE EFFECTS: The most frequent side effects are headaches, dry lips and skin, flushing, changes in blood fats (e.g. cholesterol) and decreased levels of thyroid hormone. Not everyone will experience these, but if you notice any side effects while taking Toctino, you should discuss them with your doctor, who may reduce your dose.
WARNING: Toctino is not to be taken by women who are pregnant, breastfeeding or trying to conceive. The drug can only be prescribed if a pregnancy test is negative. Regular pregnancy tests will be taken during treatment. You must avoid becoming pregnant during treatment and for 1 month after stopping treatment (e.g. by using two effective methods of contraception). Patients receiving accompanying treatment with the specific antibiotic group of ‘tetracyclines’ should not take Toctino due to the risk of the drugs interacting with each other.
Phototherapy
All you need to know about Phototherapy by clicking HERE
Phototherapy (UVB or PUVA), using either UVB or UVA rays administered by a special foot/hand light box, may be recommended if this treatment option is available locally to you. Assessment and treatment (2-3 times a week) would usually take place in a dermatology department. In some areas of the UK you may be loaned a light box so you can administer your treatment at home, although you will continue to be monitored by the dermatology department. Prior to treatment, your hands are coated in a light-sensitising solution called psoralen (the ‘P’ in PUVA). Phototherapy treatment usually continues for a few months until the eczema has resolved.

Practical tips for looking after your hands
Use a soap substitute or your usual leave-on emollient to wash your hands with, and avoid plain water. Pat your hands dry with a soft towel rather than rough paper towels, and then re-apply your leave-on emollient.
Never wash your hands with soap while wearing a ring as it can collect under the ring and cause irritation. Rings should not be worn during housework, even when the eczema has visibly healed, as cleaning products and dust can become trapped under them and irritate the skin.
When drying your hands, take special care between the fingers where the skin is more prone to dryness and cracking, and build-up of soap residue.
When washing up, use plastic or non-allergenic rubber protective gloves with cotton liners, or – even better – use a dishwasher. Try not to wear plastic/rubber gloves for more than 20 minutes at a time as they can cause the skin to sweat, which can aggravate eczema. Avoid direct contact with detergents, cleaning agents, solvents and stain removers.
Do not peel citrus fruit, onions, chillies or garlic with bare hands. Many fruits and vegetables are irritants. If you do handle them with bare hands, wash your hands as soon as possible afterwards and apply an emollient.
Wearing rings (especially those made from inexpensive metals that may contain nickel) may worsen hand eczema.
People with a history of hand eczema need to carefully consider their choice of career, as certain occupations carry the risk of contact with substances that may cause irritation and/or allergy. These commonly include: hairdressing, catering, healthcare professions, metal work, floristry, mechanics, domestic/cleaning work, some types of engineering, and printing.
Pocket Guide on Hand Eczema can be downloaded clicking HERE
